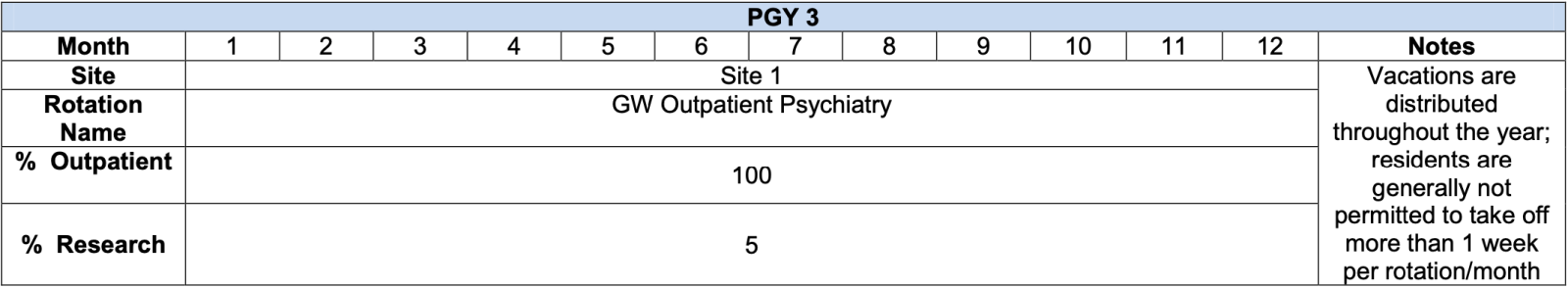
The PGY-III year is devoted to outpatient psychiatry.
Residents gain competence in long-term psychodynamic psychotherapy through a sequence of seminars, weekly supervisions with two different psychodynamic supervisors, and psychodynamic psychotherapy cases. In addition, they learn how to conduct focal psychotherapies utilizing a range of models for brief psychotherapy, each with seminars, supervisions, and assigned cases. Brief Psychotherapy adapts methods from narrative, solution-focused, interpersonal, and cognitive-behavioral psychotherapies to outpatient psychiatric treatment.
Family therapy, group therapy, and outpatient psychopharmacology are also taught with seminars, weekly supervisions, and assigned cases. PGY-III family therapy training emphasizes family interventions and family-centered care for patients with chronic medical or psychiatric disorders. Each resident also conducts a weekly group therapy with supervision throughout the year. Each resident meets weekly with a clinical psychopharmacologist who supervises medication treatments. Residents learn not only how to implement these outpatient therapies in office settings, but also how to design and implement outpatient psychiatric services that integrate these therapeutic modalities with psychoeducation and resilience-building interventions. The PGY-II consultation-liaison psychiatry rotation is supplemented by advanced PGY-III training in consultation-liaison psychiatry that focuses upon bedside brief psychotherapy with medically-ill inpatients and outpatient consultation to reproductive mental health, weight management, amyotropic lateral sclerosis, and oncology medical clinics. PGY-III residents rotate monthly journal club presentations for discussions led by GW faculty.
PGY-III residents each complete a three week full-time Residency Fellowship in Health Policy, made possible through collaboration with the GW Milken Institute School of Public Health. Mornings are devoted to lectures by national experts who cover a broad scope of topics in healthcare and public policy. Field trips occur in the afternoons to a range of sites where health policy is formulated or implemented, including the Institute of Medicine, the U.S. Capitol Congressional Office Building, National Institutes of Health, Washington “think tanks”, and public systems of healthcare within Washington. Residents conclude the rotation with group presentations of policy analyses on major health policy issues to the Deans of the GW School of Medicine and the Milken Institute School of Public Health and other invited discussants.
The PGY-III year is supervised by a broad range of different supervisors representing each of the outpatient therapies. The Outpatient Chief Resident monitors resident caseloads to ensure that each therapeutic approach is appropriately represented. PGY-III residents typically conduct:
- Long-term psychodynamic psychotherapy
- Brief individual psychotherapy
- Group therapy
- Couple and/or family therapy
- “Split-treatment” psychopharmacological treatment with patients treated in the psychotherapy clinic of the GW Doctoral Program in Professional Psychology
- Diagnostic psychiatric evaluations and psychopharmacological treatment on interdisciplinary treatment teams at neighborhood health centers and community mental health centers in the District of Columbia
PGY-III residents spend approximately 8 hours weekly in didactic seminars and clinical case conferences and approximately 5 hours weekly with supervisors representing each of the different outpatient therapies.
Seminars and Clinical Conferences
A didactic curriculum of seminars and clinical conferences parallels residents' clinical work. Teaching occurs in small groups where intimate dialogues are possible. Seminar leaders are drawn both from our full-time academic and voluntary clinical faculties, many of whom have distinguished national reputations. In general, seminar leaders employ multiple teaching modalities— lectures, live interviews of patients and families, videotaped interviews, and case reviews. Depending on resident feedback and changing trends in psychiatric education, modifications are made each year.
| PGY-III Curriculum | |
|---|---|
|
Brief and Supportive Psychotherapy |
Sexual Health |
|
Somatic Trauma Therapy for Posttraumatic and Dissociative Disorders |
Reproductive Psychiatry |
|
Clinical Psychopharmacology |
Social Neuroscience of Stigma |
|
Grant Writing, Research and Academia |
Health Policy Rotation |
|
Psychiatric Interviewing |
Family and Systems Therapy |
|
Case Conference |
Neurology for the Psychiatrist |
|
Group Therapy |
Psychotherapy Case Conference |
|
Interpersonal Psychotherapy |
Psychiatry Journal Club |
|
Hope Modules |
T-Group |
Affiliated Institutions
The McClendon Center
The McClendon Center is a District of Columbia Core Service Agency that serves the needs of approximately 700 adults diagnosed with serious and persistent mental illness. Its individualized, multidisciplinary programs seek rehabilitation of patients as persons, by fostering creativity, friendship, stability, independence, emotional growth, and greater participation in the community. The Center provides day programming, case management, psychiatric care, and counseling at two sites. McClendon Center is the only Washington, DC community mental health agency with accreditation from the Joint Commission on Accreditation of Healthcare Organizations (JCAHO). PGY-III and PGY-IV residents learn community psychiatry and mental health services delivery through their work on McClendon Center interdisciplinary treatment teams.
Pathways to Housing DC
Pathways to Housing DC is a unique community agency that specifically targets homelessness among people in the District of Columbia who are disabled by mental illnesses. Pathways for Housing has received numerous awards and commendations for the effectiveness of its innovative program, including the Gold Award from the American Psychiatric Association. Most Pathways patients have been both homeless and dually-diagnosed with mental illnesses and substance use disorders. The "housing first" Pathways model provides housing first, then supportive treatment services for mental and physical health, substance misuse, education and employment. Housing is provided in apartments scattered throughout the community. Psychiatric care is supported by ten ACT teams that make home visits and respond to crises. A walk-in psychiatric clinic is provided at the Q Street NE center. PGY-III and PGY-IV residents learn assertive community treatment and the "housing first" model at Pathways for Housing DC.
Northern Virginia Family Services
The Multicultural Human Services Program of Northern Virginia Family Services (NVFS) in Falls Church, Virginia, provides extensive community mental health services for immigrants and refugees in Northern Virginia, a region in which 180 countries and 100 languages are represented in the public schools. NVFS provides social services such as housing assistance, English as second language, job skill training, psychological assessments for refugees seeking political asylum, and mental health counseling. For over a decade, the Program for Survivors of Severe Trauma and Torture (PSTT) has been one of our nation’s major treatment programs for survivors of political torture. The PSTT program is funded by the U.S. Office of Refugee Resettlement and other humanitarian organizations.
Psychiatric services for NVFS are provided by GW psychiatry faculty, residents, and medical students. Faculty and residents treat both refugees with posttraumatic symptoms from political violence, war, or torture in their countries of origin, and immigrants with mental disorders unrelated to traumatic stress. Most clinical work is conducted with translators.
University Mental Health Center at Gallaudet University
The Mental Health Center (MHC) at Gallaudet University is located on the campus of the world's only four-year liberal arts university for deaf and hard of hearing undergraduate students. Gallaudet University offers graduate-level programs available to deaf, hard of hearing, and hearing students. In addition, summer and continuing education coursework, as well as sign language classes, are offered.
The Gallaudet University MHC's primary goal is to serve the mental health needs of a wide range of clients, both the students of Gallaudet University and deaf and hard of hearing adults in the Washington metropolitan area. Mental health services are provided by an interdisciplinary team of psychotherapists, counselors, and psychiatrists. Gallaudet MHC is a training site for graduate student-trainees in psychology, social work, and other mental health disciplines. A program of clinical research furthers an understanding for how mental health services can best respond to the problems of deafness.
Merrifield and Gartlan Mental Health Centers of the Fairfax County Community Services Board
Merrifield and Gartlan Mental Health Centers of the Fairfax County Community Services Board, operated by the Fairfax County Community Services Board, each provides a broad range of mental health services in Fairfax County, Virginia, for the treatment of mental illnesses and for prevention and early intervention to reduce incidence and severity of emotional and behavioral disorders. Their programs include emergency services, crisis intervention, forensic services, outpatient psychotherapy, medication management, community support programs, day treatment, and residential treatment. Well-funded and staffed with seasoned clinicians, they serve as model community mental health systems. GW psychiatry residents can elect PGY-III and PGY-IV advanced level community psychiatry rotations at Merrifield and Gartlan Mental Health Center.
Georgetown Ministry Center
Georgetown Ministry Center guides service-resistant, chronically homeless individuals towards stability and housing through aggressive street outreach, provision of a safe and welcoming environment where everyone is treated with respect, and advocacy for the homeless. They seek lasting solutions to homelessness one person at a time. GMC has grown to include a successful drop-in center, street outreach, and a winter shelter that offers a safe haven from the streets to our most withdrawn and vulnerable population. GMC’s unique presence in Georgetown makes us an essential part of the net of services cast to the city’s homeless population. At Georgetown ministries, our residents provide comprehensive psychiatric care for the DC’s most vulnerable population. Psychiatry residents receive training in community psychiatry, with an emphasis on ACT team model, in which the residents go into the community to provide psychiatric care.